|
I recently attended a lecture, hosted by the Nipissing Naturalists Club on the topic of the Black Legged Tick, given by Dr. Katie Clow from the University of Guelph. Dr. Clow has been in the Nipissing area studying our tick population, which is pretty cool! What do you need to know? Well, first of all, the basics. Lyme Disease is caused by a bacterial spirochete carried by ticks. The most famous bacterial spirochete causes Syphilis. Ticks carrying Lyme Disease have been gradually moving into Ontario, current hot spots include the shores of Lake Erie and Lake Ontario, along the St. Lawrence River, Thunder Bay, and the Kingston area. As the climate changes, ticks are expected to move further and further north, supported by warmer temperatures and sometimes carried by migratory birds. Because birds can drop ticks anywhere, you can become infected by Lyme Disease in our area, although it is currently highly unlikely. Here are some basic facts, as presented by Dr. Clow:
Click here for more information about how to protect yourself from ticks and what a Lyme disease infection might look and feel like. [Credit is also given to the Ontario Ministry of Health and Long-Term Care and the CDC for the photo used at the top of this post.]
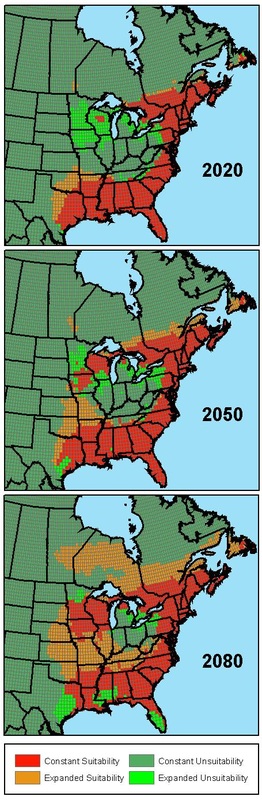
Here is the information released to the public by the North Bay Parry Sound District Health Unit. "In 2013, 21 ticks were submitted through human exposure for identification, two specimens were not ticks and nine specimens were identified as Ix. scapularis, the species of concern for the transmission of [Lyme Disease]. The results for seven of the nine specimens were negative for B. Burgdorferi, the agent for [Lyme Disease]. At the time this report was written, the results for two specimens were still pending from the Public Health Agency of Canada lab. In 2013, 311 cases of [Lyme Disease] were reported in Ontario. This is a substantial increase from 2012, when 101 cases were reported (Public Health Ontario, 2013). There was one positive human cases of [Lyme Disease] in the [North Bay Parry Sound District Health Unit] area in 2013." (Elsewhere in the report, they specify the positive case in 2013 was travel-related) We can expect Lyme Disease to eventually become more common in our area (see the image below). This image is a projection of Black Legged Tick expansion based upon climate change projections using the 'Canadian Global Coupled Model' taken from the 2005 publication Effect of Climate Change on Lyme Disease Risk in North America. What Do I Need to Know About Lyme Disease Testing and Treatment? The easiest way for a medical doctor, naturopathic doctor, or nurse-practitioner to diagnose Lyme disease is clinically, based on a combination of the following factors: 1) exposure to the outdoors in an area where Lyme Disease is endemic, and 2) the characteristic bull's-eye rash, and/or 3) symptoms such as fever, diffuse rash, and muscle aches. If you aren't being diagnosed based on this criteria, you suspect you have Lyme disease, and the tests your medical doctor or nurse practitioner have run are not coming back positive, you can speak to a naturopathic doctor about more extensive testing. The most important thing is to get tested as soon as possible. Your ideal testing window is in the first six weeks after you are infected. The second thing you need to know is that antibiotics are the ideal treatment immediately after infection. The current research suggests the ideal duration of antibiotics after a recent infection is 10 days, though this is a bit of a controversial topic. You should definitely ask for more than one day of antibiotics, if this is the prescription you receive. Chronic infections (see below) require different protocols, and benefit tremendously from the inclusion of naturopathic care. The Stages of Lyme Disease It is a common theory that Lyme disease can become chronic if not caught early and/or treated successfully. Some patients report that their Lyme disease was not successfully eradicated with the recommend course of antibiotics. Many people do not develop the characteristic bull's eye rash (if they develop any rash at all), meaning the disease would not necessarily be detected in the acute stage. Chronic Lyme disease is believed to evolve into problems with arthritis and the neurological system, in particular. You can learn more here. Resources:
http://myhealthunit.ca/en/partnerandhealthproviderresources/resources/2013_NBPSDHU_Vector_Borne_Diseases_Report.pdf http://canlyme.com/ http://www.igenex.com/Website/# http://www.health.gov.on.ca/en/public/publications/disease/lyme.aspx Clinical Key - First Consult - Lyme Disease - Revised: 18 Jul 2013 http://www.ncbi.nlm.nih.gov/pubmed/20070237
1 Comment
|
AuthorDr. Dielle Raymond, ND Archives
March 2020
Categories |
This website is intended for educational purposes only. There are no contents on this website that are intended to provide medical advice, diagnosis, or treatment. Copyright ©2023 Dr. Dielle Raymond, ND. All Rights Reserved.


 RSS Feed
RSS Feed